Venter Institute Researchers Tackle the Growing Concern of Antibiotic Resistant Bacterial Infections with Genomic, Phage Approaches
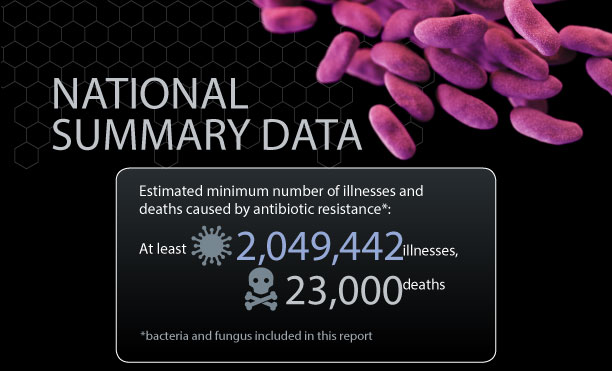
The Centers for Disease Control and Prevention (CDC) estimates that each year in the United States two million people acquire antibiotic resistant bacterial infections that lead to 23,000 deaths. Antibiotic resistance affects people of all ages and seriously impacts the healthcare, veterinary, and agriculture industries, making it one of the world’s most urgent public health crises. Because of this, the CDC has labeled certain multidrug-resistant bacteria, “superbugs.”
Derrick Fouts, PhD, Professor in the Infectious Disease Group at JCVI, leads a team exploring relationships between bacterial genetic variation, emergence of antibiotic resistance, and how this intersection affects patient outcomes.
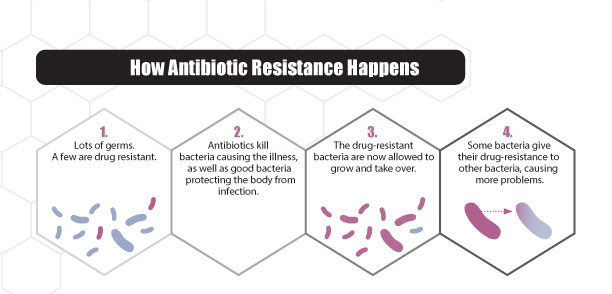
Ever since penicillin, the first commercially available antibiotic, drug resistance has evolved alongside new antibiotics. Bacteria are constantly developing new ways to resist drugs and sharing their resistance with one another, making the race towards improved antibiotics, critical.
No one can completely avoid the risk of antibiotic resistant infections, but people with chronic illnesses are most susceptible. Further complicating this growing health epidemic, chronic illnesses affect approximately 133 million Americans, representing more than 40% of the total population. Very few drugs with activity against multidrug-resistant organisms (MDROs) have been brought to market—fewer still are expected in the foreseeable future—therefore, novel and alternative countermeasures are needed.
The JCVI team, in collaboration with Dr. Josh Thaden and Vance Fowler of Duke University Medical Center, is using clinical information from the Bloodstream Infection Biorepository (BSIB), provided by Duke University, in conjunction with whole genome sequencing to identify associations between bacterial genotypes and poor clinical outcomes.
The team’s objectives ultimately are to lower in-hospital mortality rates, complications of blood stream infections (BSI) such as septic shock, acute kidney injury (AKI), acute lung injury (ALI)/acute respiratory distress syndrome (ARDS), disseminated intravascular coagulation (DIC), and ischemic liver injury.
Through genomic-based epidemiology, the team is developing enhanced molecular tools to help physicians identify patients with particularly hard to treat infections, leading to more informed and improved treatment plans.
To address the problem of antibiotic resistant bacteria directly, Dr. Fouts and co-investigator Sanjay Vashee, PhD, are utilizing synthetic genomics techniques to design and engineer bacteriophages (or phages) to combat antibiotic resistant infections.
Phage are viruses that only infect bacteria and are not harmful to humans. In phage therapy cultures of infectious phages are used to treat bacterial infections, which has the advantage over antibiotics because the phage target specific bacterial species or strains while multiplying and spreading to infect more target bacterial cells.
Phage therapy became very popular throughout the world in the early 20th century to treat a wide range of diseases caused by a variety of bacterial pathogens. After the discovery and production of penicillin for use during World War II, phage therapy fell out of favor in many western countries, particularly the US.
The phage therapy cocktails used in the past didn’t always work and some of that had to do with phage strain selection and bacteria developing resistance to them. Today, though the use of synthetic genomics techniques and tools, standardized cocktails of phage can be rapidly and efficiently engineered to be more clinically effective than traditional phage cocktails created by mixing phage isolated from sewage.
Through their work, the JCVI team believes novel phage products can be developed that could lead to improved prevention and treatment for MDRO infections where few treatment options remain due to the spread of multidrug-resistance. Potential treatments would include topical creams or wound dressings with the bacteriophage drugs in them. This work could also lead to new disinfecting agents to remove these MDROs from hospital equipment and surfaces; thus, preventing the risk of spread of these infection-causing bacteria.