Unique Antibody Pattern Discovered in COVID-19 ICU Patients May Be Key to Predicting Severe Outcomes
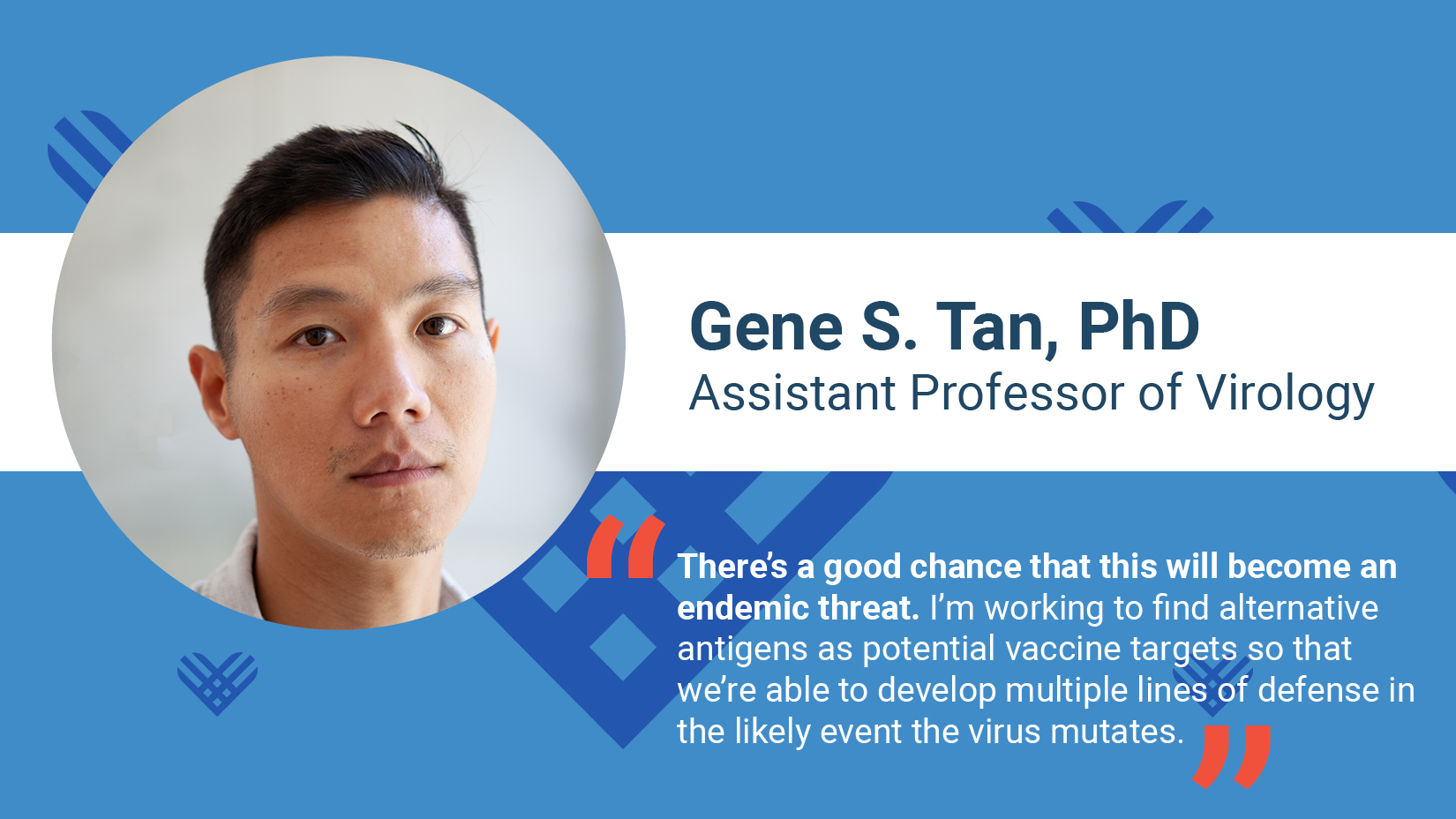
While news of promising COVID-19 vaccine trials is heartening, the fight to control infection rates and develop effective treatments will be an ongoing challenge for science for years to come. Gene Tan, PhD and his collaborators are working on identifying testing models and tools that will allow more labs to safely work on the disease, identifying varying inflammatory responses to the disease for more targeted testing and treatment plans, and identifying additional viral targets to anticipate the likely mutation of the virus and future vaccine development.
Research into new emerging and highly infectious agents like SARS-COV-2 are rightly conducted in highly secure labs when the research involves live virus, which ensures safety and containment. However, much of the genomic research of today can be done without using live virus and thus biosafety labs at the highest level are not needed. But not all labs have the necessary tools and testing models, which is where Dr. Tan and his collaborators come in. They are developing tools and safe testing models that will be more plentiful and available to a variety of labs, which will help lead to more discoveries in vaccine development, patient testing and therapeutics.
Dr. Tan and his collaborators are also researching the different levels of immune response to the disease, particularly in men, that translates into varying levels in severity of the disease. Many Individuals are displaying a heightened immune response, while normally beneficial to fighting off disease in general is actually leading to severe symptoms and putting more patients in the ICU.
An antibody is a Y-shaped protein used by the immune system to identify and fight pathogens such as harmful bacteria and viruses when they enter our body. This Y shaped structure allows antibodies to carry out their dual functions. Each tip of the Y is responsible for binding to specific antigens of the pathogen and tagging it for attack by other parts of the immune system or neutralizing it directly. The base of the Y, called the Fc region, is responsible for communication with the immune system and modulating immune cell response, and it is this part of the antibody elicited by SARS-CoV-2 infection that Dr. Tan and his collaborator, Dr. Taia Wang at Stanford University, have been closely monitoring. They discovered that while the relative quantitative antiviral antibody titers are similar between different patients, the glycosylation pattern of the Fc is different in people who have severe disease. The data suggest that there is a qualitative difference in the antibody responses associated with a higher inflammatory response translating to the severity of symptoms that one may develop. Dr. Tan is also working with Dr. Marcelo Freire, another investigator here at the J. Craig Venter Institute in a parallel study – where we are currently characterizing the antibody response to SARS-CoV-2 in the human salivary fluids.
The overarching goal is to understand the mechanisms by which the immune system successfully promotes the clearance of the virus infection or results in more severe disease due to an over active inflammatory response. Understanding the basis of these pathways will allow us to identify high-risk patients easier, as well as identifying personalized and more effective treatment plans.
The current vaccines in clinical trials are focusing on one viral antigen. While this is a good plan for targeting the current iteration of the disease, the virus may develop mutations, much like seasonal influenza. Capitalizing on his long history of working on improving influenza vaccine efficacy, Dr. Tan is investigating additional disease antigens as potential vaccine targets which can lead to increased efficacy and broader protection.