Influenza: Host-Virus-Microbiome Interactions
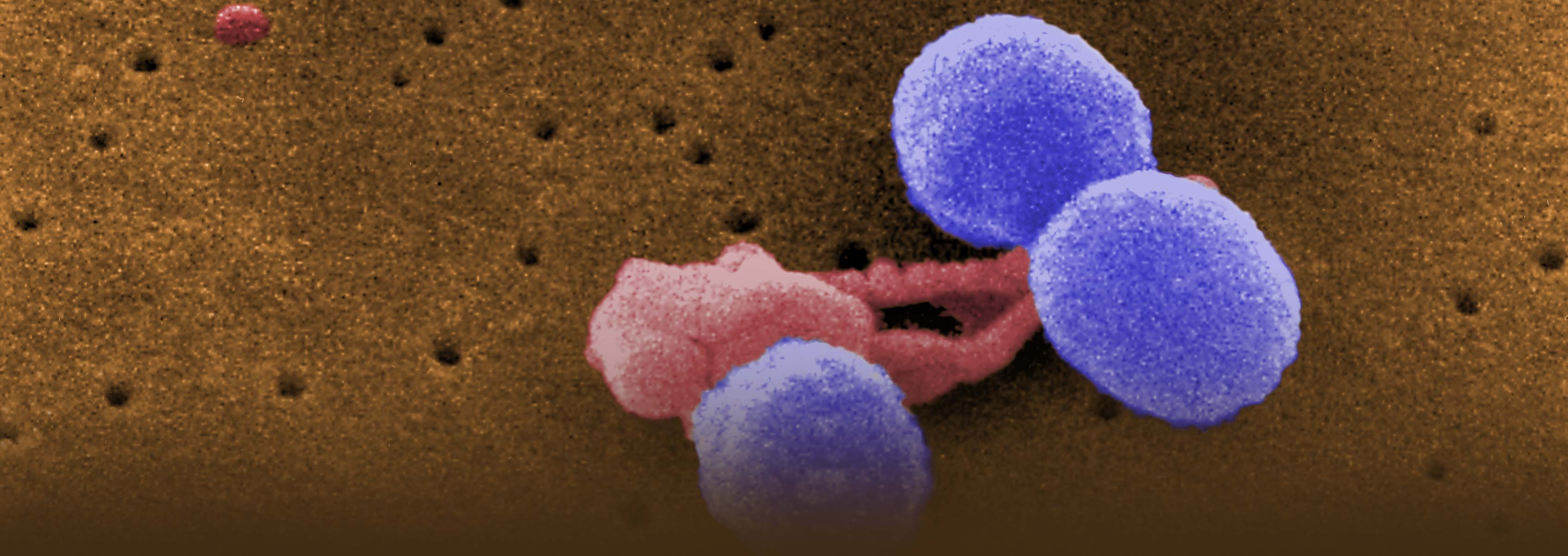
Influenza is a leading cause of death in the United States and worldwide, resulting in approximately 40,000 deaths annually due to seasonal epidemics alone. A major complication of influenza infections resulting in lethality, particularly during pandemics, is secondary bacterial infections of the lung (pneumonia). Streptococcus pneumoniae, Staphylococcus aureus (especially methicillin-resistant S. aureus or MRSA), and Hemophilus influenzae are the most common pathogens associated with secondary bacterial infections, although other bacteria (e.g., Chlamydia, Klebsiella, etc.) are clinically observed. The mechanisms responsible for secondary bacterial infections are poorly understood, and currently, clinicians lack the ability to identify individuals at risk (let alone intervene therapeutically) for this deadly complication.
Bacterial colonization of the upper respiratory tract (e.g., nasal passages) frequently precedes the development of bacterial pneumonia, but how viral infections alter the microbial composition of the upper respiratory tract has not been investigated. Animal data from murine models of sequential influenza and bacterial infections suggest that either the viral infection itself or activation of the antiviral immune state enhances the susceptibility to bacterial infection of the lower respiratory tract (i.e., pneumonia), but this has yet to be examined in human patients. Since the nose is the main portal of entry for respiratory viruses, this location serves as a logical and easily accessible site for analyzing how viruses or host antiviral immune responses induce changes in the nasal microbiome, which may predict risk of secondary bacterial pneumonias. This comparative analysis of the microbial diversity found in the nasal passages of normal and influenza-infected individuals will provide insights into the interactions between commensal and pathogenic bacteria, as well as elucidate how viruses alter these relationships and enhance risk of secondary infections. To address these questions, we plan to study nasopharyngeal (NP) samples from individuals over the course of an IAV infection. To rule out co-infections, all influenza-positive samples will be analyzed by a commercially available RT-PCR test against 14 common respiratory viruses. The proposed sequential sampling will allow us to evaluate the 16S profiles, viral infection kinetics (titers), viral genotypes, and intra-host diversity over the course of a human IAV infection.
Funding
Research reported in this publication was supported by the National Institute Of Allergy And Infectious Diseases of the National Institutes of Health under Award Number U19AI110819. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.